Could what the eyes see be misleading?
A comparison between the manufacturers’ recommended manual cleaning of endocavity and surface ultrasound probes and the fully automated reprocessing of the same ultrasound probes with Ethos® Automated Ultrasound Probe Cleaner Disinfector.
It is essential to remember, as outlined in the Spaulding classification system, that reusable medical devices, including ultrasound transducers or probes, must be cleaned and subsequently disinfected between each patient to prevent the spread of infection. Proper cleaning of ultrasound probes is essential for promoting patient safety, maintaining probe functionality, and preventing healthcare-associated infections (HAIs). Cleaning is the process of removing debris and foreign material from an ultrasound probe, and it is a crucial step in the high-level disinfection process. Ultrasound probes can come into contact with multiple non-sterile patient tissues, potentially contaminating the probes with microorganisms. The cleaning process can remove 4-6 log10 bacteria from contaminated medical devices (1-4). Reductions in bacterial numbers on contaminated devices promote bacterial killing during subsequent high-level disinfection, as lower numbers of microorganisms are easier to kill with disinfectants compared to higher concentrations. The physical removal of debris is also crucial to ensure proper high-level disinfection, as soil and debris can inhibit or inactivate some disinfectants (5-6) and/or protect microorganisms from being killed by the disinfectant (2, 7, 8). Inadequate bacterial killing on ultrasound probes can promote the formation of biofilms, which are groups of microorganisms that live together and are protected by an extracellular matrix. Bacterial biofilms are more difficult to remove with cleaning and are more resistant to killing by disinfectants than free-living bacteria. Thus, the need for proper cleaning prior to disinfection is instrumental in providing safe, disinfected probes for use in clinical procedures.
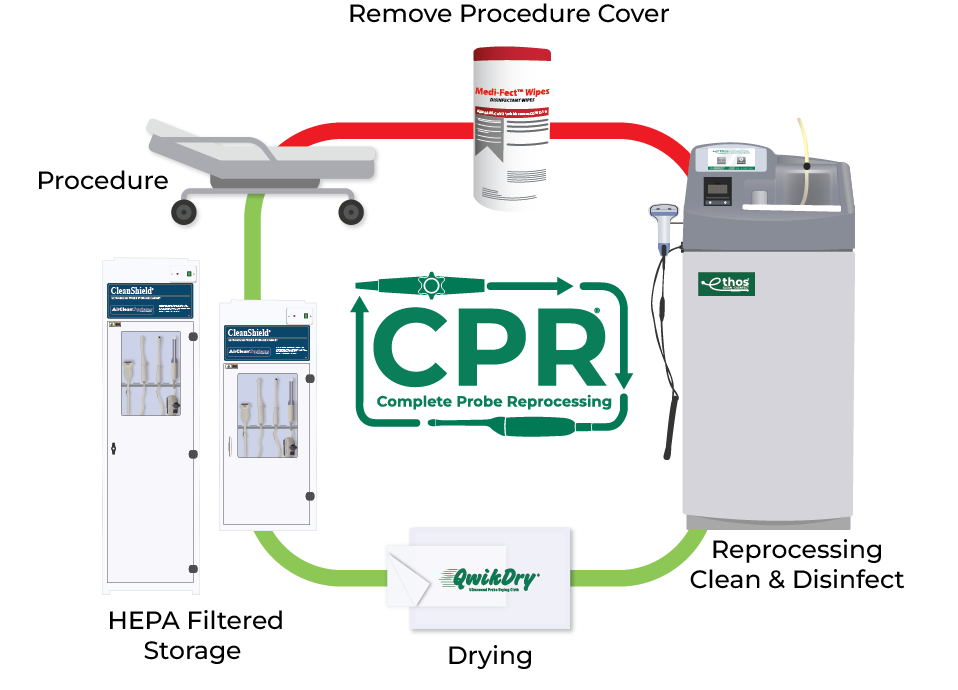
Reprocessing with Ethos
A standardized, evidence-based guidelines approach to the reprocessing of endocavity & surface probes improves quality, reduces variations, and controls cost in a variety of areas, from patient care to supply chain to overall departmental revenue management.
References:
- Alfa, M.J., P. Degagne, and N. Olson. "Worst-case soiling levels for patient-used flexible endoscopes before and after cleaning." American Journal of Infection Control, 1999. 27(5): p. 392-401.
- Rutala, W.A., D.J. Weber, and H.I.C.P.A. Committee. "Guideline for Disinfection and Sterilization in Healthcare Facilities", C.f.D.C.a. Prevention, Editor. 2008. p. 14-21.
- Chu, N.S., D. McAlister, and P.A. Antonoplos. "Natural bioburden levels detected on flexible gastrointestinal endoscopes after clinical use and manual cleaning." Gastrointestinal Endoscopy, 1998. 48(2): p. 137-142.
- Hanson, P.J., et al. "Recovery of the human immunodeficiency virus from fibreoptic bronchoscopes." Thorax, 1991. 46(6): p. 410-412.
- Lambert, R.J. and M.D. Johnston. "The effect of interfering substances on the disinfection process: a mathematical model." J Appl Microbiol, 2001. 91(3): p. 548-55.
- Rutala, W.A. and D.J. Weber. "Uses of inorganic hypochlorite (bleach) in health-care facilities." Clin Microbiol Rev, 1997. 10(4): p. 597-610.
- Lewis, D.L. and M. Arens. "Resistance of microorganisms to disinfection in dental and medical devices." Nat Med, 1995. 1(9): p. 956-8.
- Muscarella, L.F. "Sterilizing dental equipment." Nature Medicine, 1995. 1(12): p. 1223-1224.